Article
Initial Diagnostic Assessment

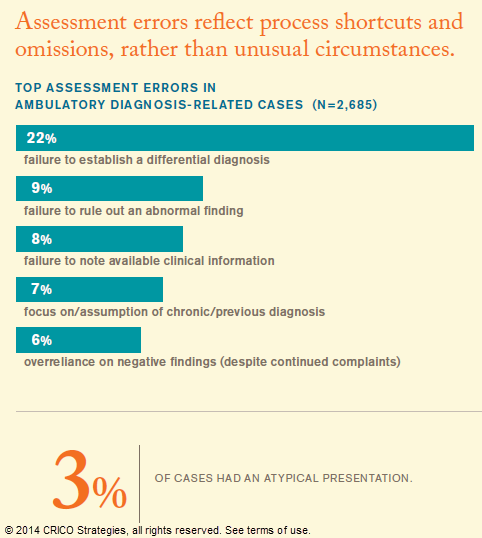
More than half of the cases analyzed for Candello’s 2014 Benchmarking Report: Malpractice Risks in the Diagnostic Process, reflect missed opportunities early in the diagnostic process, before and during the formation of a differential diagnosis. This is when physicians determine whether to rely on instinct or which tests, if any, should be ordered. This is also when the risk of a missed or delayed diagnosis is highest.
What physicians have seen most often, and most recently, can bias how they weigh the current evidence. The terminology around the failure to establish a differential diagnosis is well known: anchoring, cognitive framing, premature closure, and most commonly, narrow diagnostic focus. It is also, of course, what works for the vast majority of patient encounters. Physicians see patterns because they are there. They employ diagnostic heuristics because they are efficient. In addition to the confidence of experience, physicians are challenged by the tension between utilization and productivity. A belief that excessive probing and expanding the differential is unlikely to further benefit the patient in the exam room (and will irritate those in the waiting room) has to be balanced against the assuredness that enough information is in hand.
Unfortunately, missing pieces of the diagnostic puzzle can trip even the most accomplished providers. Without an updated family history, a comprehensive exam, and a thorough review of the medical record, a physician with the right intentions can make a wrong decision. Discounting symptoms or signals that don’t support the diagnostic hypothesis (she’s too young, it’s just hemorrhoids, he’s a big eater) puts patients and providers at risk of missing elusive, but not necessarily rare, diagnoses.
Analysis of missed opportunities during the initial assessment indicate that applying some universal practice standards might have illuminated what the clinicians failed to see: updating the family history, listening to the patient’s complete story, expanding—then narrowing—the differential diagnosis, asking what non-supportive labs or test results could be revealing. Often, physicians who respond to internal or external pressure to make a diagnosis—despite absent or contrary indicators—later regret not having kept the diagnostic process open until they had more supportive information in hand.
Dr. Hardeep Singh discusses how doctors can experience calibration (overconfidence when you think you are right) in diagnosing patients. (20 sec)
Lack of appreciation for significant elements of the patient’s history and physical led to a missed PE.
This page is an excerpt of the full Candello report: Malpractice Risks in the Diagnostic Process.
Diagnostic Process Report Contents
Related Articles
Are You Safe?

Closed Case Abstract: Sleep Apnea Patient Dies After Eye Surgery

Resources for Presenters