Article
Malpractice Risks Associated with Electronic Health Records
The full potential of health information technology (health IT) has not yet been realized, and of particular concern are the examples of unintended consequences of health IT that detract from the safety of health care. The goal of this study was to obtain additional information on these health IT-related problems using a mixed methods (qualitative and quantitative) analysis of electronic health record (EHR) related harm cases submitted to CRICO Strategies Comparative Benchmarking System (CBS).
CBS is a national database representing nearly 400,000 malpractice suits and open and closed claims from captive and commercial insurers representing more than 400 hospitals and health care organizations.
Methodology
A retrospective, cohort study of claims in the CRICO Strategies national Comparative Benchmarking System was conducted for medical malpractice cases coded using a specific coding taxonomy during the period January 1, 2011, through December 31, 2015. Cases selected for this analysis were open and closed malpractice claims and suits with one or more EHR identifiers as a contributing factor in the case.
Outcomes/Failures Occur When...
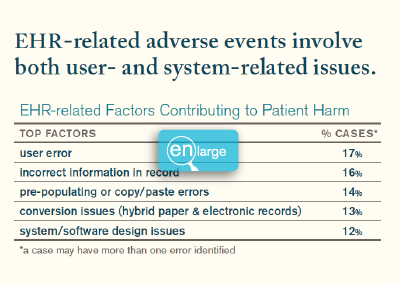
The data in this study confirms that adverse events related to using electronic medical record systems exist, that they are associated with an appreciable incidence of severe harm and death, that they are encountered across the continuum of health care settings, and they involve both human and technical issues/failures. The top five factors that account for half of the EHR-related cases in this study, include user error, incorrect information in record, pre-populating (copy/paste errors), conversion issues and system issues.
System-related issues involve technology and design issues. Examples include:
- PCP cannot access radiology studies during patient visit; results later filed without PCP review. Result: delayed diagnosis of lung cancer.
- MD unable to access nursing ED triage note. Result: death from mismanaged subarachnoid hemorrhage.
- When the complaint field was too small to record “sudden onset chest pain w/burning epigastric pain,” the patient’s complaint was shortened to “epigastric pain.” Result: mismanaged workup and subsequent cardiac event.
User-related issues include training and education. Examples include:
- OB could not access patient’s clinic notes documenting abnormal fetal size, citing lack of training and no EHR password.
- MD received an amoxicillin allergy alert but ordered it anyway, causing allergic reaction.
- Patient developed amiodarone toxicity after history and medications copied from previous note did not document patient was already on this medication.
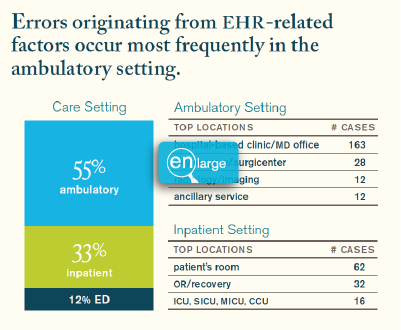
Issues related to EHR were found to be more prevalent in the ambulatory setting (55%) with 39% of these cases resulting in a high severity outcome.
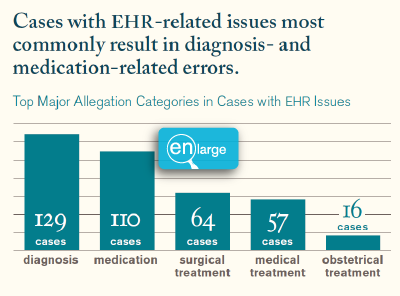
Diagnosis and medication related allegations are most common in cases with EHR-related events.
Medicine, surgery, and nursing are the most noted services in cases with EHR-related issues. The data also demonstrate that ED-based EHR-related errors result in more significant patient harm (57%) compared to EHR errors in the inpatient setting (45%) and ambulatory setting (39%).
Conclusion/Solution
Electronic health records serve a critical role in the delivery of safer care allowing ready access to coordinated medical records, decision support, clinical alerts and follow-up/screening reminders but it is not without vulnerabilities. Medical malpractice data provides a unique lens into these vulnerabilities by identifying the contributing factors associated with these events. Electronic health record events rarely stand alone and can cause extensive harm. They are encountered across the continuum of health care settings and must be understood in the context of broader system breakdowns and care failures.
Next steps should include organizational-wide responses that embrace the EHR as an integral part of risk and patient safety programs along with a system-wide awareness/education around the vulnerabilities in EHR use. There should be IT, vendor, and clinician collaboration to understand provider needs to improve system design and function.
Related Articles
Navigating Risks in Breast Cancer Diagnosis and Treatment


Opening Your Notes: Patient Care Recommendations