Article
Neurosurgery and Medical Malpractice Risk
Of all the physician specialties, neurosurgery is arguably the one most impacted by medical malpractice claims. An analysis of paid malpractice claims from the National Practitioner Data Bank over the period 1992–2014 found that neurosurgeons had the highest incidence of paid malpractice claims, at 53.1 claims per 1000 physician-years, and the largest average malpractice payment, at $469,222.1 A more recent analysis of malpractice claims, which was based on data from the Westlaw database, found that, for neurosurgery cases on which an indemnity payment was made, the median payments were $2.55M for plaintiff verdicts and $1.3M for settlements. Among pediatric neurosurgery cases with plaintiff verdicts, the median payment was an astounding $10.1M.2
One factor behind the large indemnity payments in neurosurgery claims is that a component of the awards is for payment of future medical expenses. Therefore, when there is severe neurological injury requiring extensive ongoing medical care—especially in younger patients—the costs for such care will be high, and this is reflected in the size of the indemnity payments.
Unresolved malpractice cases can weigh on physicians, and this is another area that demonstrates the impact of malpractice on neurosurgeons. Neurosurgeons spend more than a quarter of their careers with an open malpractice claim, more than any other physician specialty. This compares to just over 10% for physicians overall.3
Beyond the numbers, a recent report in the Journal of Neurosurgery described the health effects of being named in a malpractice claim on two neurosurgeons. One suffered a fatal pulmonary embolism during the trial. Another had a non-fatal coronary and then peripheral vascular thrombotic event around the time of the trial, with subsequent recovery.4 Albeit extreme examples, these cases are emblematic of the stress that can accompany being named in a medical malpractice claim.5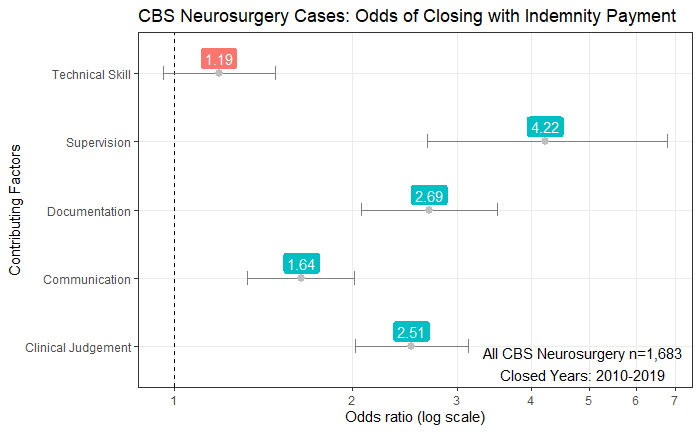
Analyses of data from malpractice cases are one tool to enhance patient safety and reduce the risk of adverse events that might give rise to future malpractice cases against neurosurgeons. Using data from Candello database, which contains roughly 30% of all malpractice claims, we determined the odds ratios that a malpractice claim will close with an indemnity payment. Based on an analysis of 1,683 neurosurgery cases, these odds ratios help identify areas that are ripe for patient safety interventions.
Interestingly, issues with technical skill did not prove to be a statistically significant predictor of which neurosurgery cases will close with an indemnity payment. Instead, the contributing factor with the greatest odds ratio was issues related to supervision. The analysis shows a case with supervision-related issues is 4 times more likely to close with an indemnity payment when compared to cases without such issues. Another significant contributing factor was problems with communication.
An example of a data-driven patient safety intervention addressing both these areas was the development of a list of critical inpatient event triggers that required the surgical resident physicians to contact their supervising attending physicians. This list of triggers included transfer to the ICU, significant neurologic changes, and the need for a blood transfusion, among others. In a study by Arriaga et al., the implementation of this program requiring notification of the attending for these critical inpatient events resulted in the percent of critical events in which the attending was not notified dropping from 33% to 2%. When residents spoke with their attendings about a critical event, one-third of the time that conversation resulted in a change in the care of the patient, highlighting the importance of this supervisory communication.6
Harnessing the power of malpractice data to identify key patient safety vulnerabilities can guide the development of programs aimed at reducing the risk of adverse events. By decreasing the risk of adverse events, we can, most importantly, avoid patient harm, and also reduce the incidence of malpractice claims against neurosurgeons—and all physician specialties.
References:
- Schaffer AC, Jena AB, Seabury SA, Singh H, Chalasani V, Kachalia A. Rates and characteristics of paid malpractice claims among U.S. physicians by specialty, 1992-2014. JAMA Internal Medicine. 2017;177(5):710-718.
- Thomas R, Gupta R, Griessenauer CJ, et al. Medical malpractice in neurosurgery: A comprehensive analysis. World Neurosurgery. 2018;110:e552-e559.
- Seabury SA, Chandra A, Lakdawalla DN, Jena AB. On average, physicians spend nearly 11 percent of their 40-year careers with an open, unresolved malpractice claim. Health Affairs. 2013;32(1):111-119.
- Maroon JC. Catastrophic cardiovascular complications from medical malpractice stress syndrome. Journal of Neurosurgery. 2019:1-5.
- Rappaport DI, Selbst SM. Medical errors and malpractice lawsuits: Impact on providers- Part 2 of 6. Pediatric Emergency Care. 2019;35(6):440-442.
- Arriaga AF, Elbardissi AW, Regenbogen SE, et al. A policy-based intervention for the reduction of communication breakdowns in inpatient surgical care: Results From a Harvard Surgical Safety Collaborative. Annals of Surgery. 2011;253(5):849-854.
Related Articles
Risks in General Medicine: Contributing Factors


Reducing the Occurrence of Malpractice Cases Involving Inadequate Patient Assessment

What’s My Risk Library