Guideline
Early Warning System Algorithm

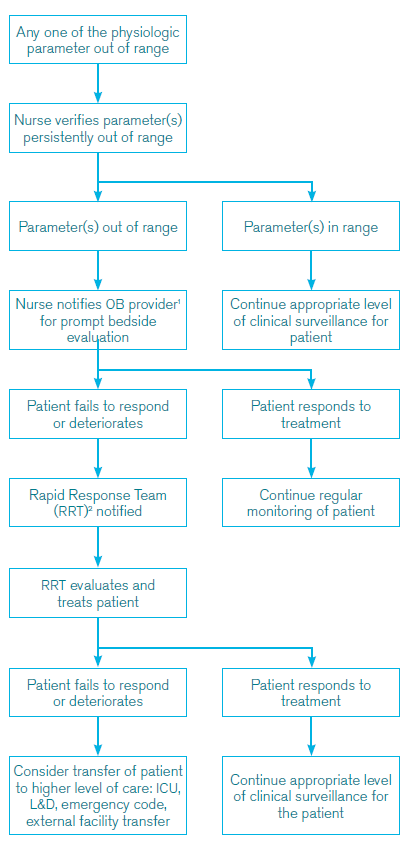
The Early Warning System algorithm identifies prompts for bedside assessment by providers with the ability to activate resources required for diagnostic and therapeutic interventions. Escalation of concern may be initiated by any team member at any point in the patient’s care.
Early Warning System Triggers
Patients may exhibit physiological changes that signify deterioration. These changes, or triggers are included in this guideline.
| MEWS TRIGGER CRITERIA* | |
| Parameter | Value |
| systolic BP (mm Hg) | <80 or >160 |
| diastolic BP (mm Hg) | >105 |
| heart rate (beats per min) | <50 or >120 |
| respiratory rate (breaths per min) | <10 or >30 |
| oxygen saturation % (room air, at sea level) | <95 |
| oliguria (mL for >2 hours): for catheterized patients | <30 |
| agitation, confusion, unresponsiveness | if any present |
| preeclampsia, with patient reporting non-remitting headache or shortness of breath | if any present |
About Early Warning System Algorithm
Over the past decade there has been an increase in birthing person mortality. Improving systems to recognize and treat early indicators of complications may prevent or reduce the severity of these situations. To that end, the CRICO OB Quality and Safety Task Force has developed Early Warning System guideline and algorithm to aid in early recognition and treatment of potentially critical complications in postpartum birthing people.
Purpose and Goal
Efforts to mitigate the severity of adverse events and ultimately improve outcomes require prompt recognition of and response to critical changes in the birthing person condition. The American College of Obstetricians and Gynecologists (ACOG) committee opinion on Preparing for Clinical Emergencies in Obstetrics and Gynecology (2014) noted over the last decade there was a 75% increase in severe birthing person morbidity from complications of delivery in the United States. Claims data from the Candello database has revealed the incidence of birthing person death cases between assert years 2009–2013 was 5.1 deaths per 100K births with a total incurred loss of over $650,000 per claim.
This document provides guidelines for developing a birthing person Early Warning System for inpatient Obstetrics (OB). The accompanying algorithm outlines the response to a decline in an obstetrical patient’s condition outside of the operating room, with the goal of preventing continued deterioration and facilitating a coordinated response, with effective communication among providers.
Birthing person mortality reviews demonstrated a significant number of cases in which abnormal vital signs preceded a critical deterioration in patient condition. An effective early warning system, with prompt bedside evaluation may facilitate timely recognition, evaluation and treatment for obstetrical patients developing critical conditions such as hemorrhage, hypertensive crisis and sepsis.
Expectations
Each institution should develop an Early Warning System, incorporating the principles within this document. Institutional leadership should provide necessary resources for implementation, including staffing, education, a quality improvement process, and leadership from senior medical and nursing personnel.
Guidelines for Implementation
- Education and training in Early Warning System triggers for clinical staff including physicians, nurses, patient care assistants, and unit support staff.
- Identification of bedside responders to an Early Warning System trigger
- Effective communication: whom to notify, how to notify them, and when and how to activate the chain of command to ensure an appropriate response.
- Identification of a Rapid Response Team to support bedside responders
- Implementation of quality improvement metrics based on the individual institution’s resources.
- Leadership support for chain of command policy to provide prompt bedside evaluation and treatment.
Staff Requirements
The initial OB provider for patient assessment should be credentialed in obstetrics and may be a physician, certified nurse midwife, nurse practitioner or physician assistant. If no credentialed obstetrics provider is available, each institution should specify an appropriate initial bedside responder, while simultaneously contacting the obstetrical attending physician.
A Rapid Response Team (RRT) is composed of clinicians that bring critical care expertise to the patient. At a minimum, an RRT should include the obstetrical attending physician, anesthesiologist covering obstetrics, and charge nurse. This team will assist in stabilizing the patient and determining when transfer to a higher level of care is indicated.
Footnotes
- OB-MD,CNM, NP, PA. If OB provider (OBP) not in facility, identify bedside responder while awaiting OBP.
- Charge nurse, OB attending, OB anesthesia attending
All members of the OB team and roles/responsibilities should be determined locally.
*Specific Early Warning System triggers may evolve as more evidence becomes available.
References
- Preparing for clinical emergencies in Obstetrics and Gynecology. ACOG Committee Opinion No. 590, March 2014, Reaffirmed 2018. American College of Obstetricians and Gynecologists.
- Mhyre JM. The maternal warning criteria. Obstetrics and Gynecology. 2014;124:782–86.
OB Quality Task Force
Thomas Beatty, MD (Co-chair)
Newton-Wellesley Hospital
Lisa Dunn-Albanese, MD
Newton-Wellesley Hospital
Fred Frigoletto, MD
Massachusetts General Hospital
Toni Golen, MD
Beth Israel Deaconess Medical Center
Kate Harney, MD
Cambridge Health Alliance
Lisa Heard, RN (Co-chair)CRICO
Ron Marcus, MD
Beth Israel Deaconess Medical Center
Alyson Preston MD
North Shore Medical Center
Brian Price, MD
Atrius Health
Julian Robinson, MD (Co-chair)
Brigham and Women’s Hospital
More CRICO Guidelines or Algorithms
General Informed Consent Guidelines


Challenge: Take the OB Clinical Guidelines Test

OB Guideline 15: Assessment and Monitoring in Labor and Delivery

