Newsletter
Documentation Best Practices
Jun 01, 2013
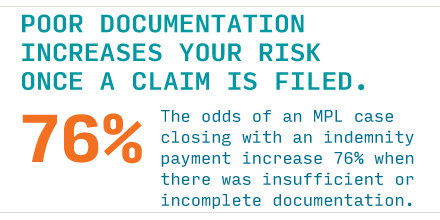
Write it Right
Protect your patients, your team and yourself by following these guidelines when writing your clinical notes.
Entries should be...
...OBJECTIVE
- Document your clinical rationale at critical decision points, e.g., a new finding or change in the patient’s condition. If appropriate, note the reason for diverging from standard practice
- Record the risk-benefit analysis of important decision.
- Don’t chart a symptom without documenting your response (response should meet the standard of care).
- Describe actions of the patient rather than labeling behavior: “pt has not kept scheduled appointment with GI” rather than “pt is difficult and non-compliant.”
- Avoid comments that could be viewed as disrespectful or prejudicial, e.g., attention seeking, histrionic, dramatic.
- Include socioeconomic information only if relevant to care.
- Document communication with other clinicians (if they are specific to the patient).
- Document patient education, instructions
- In addition to the patient, consider the “audiences” that may have access to patient records such as insurance companies, regulatory agencies.
- Avoid hearsay: do not record what someone else said, heard, felt, or smelled unless information is critical; use quotations and attribute remarks accordingly.
...SPECIFIC
- Avoid vague terms; e.g., write “9 x 5 x 1 cm wound” rather than “medium wound.”
- Beware copying and pasting review what is being copied to avoid perpetuation of information that is no longer accurate or relevant.
...TIMELY
- Notes should be recorded contemporaneously with medical care; a long time lapse before entry diminishes credibility.
- Late entries are appropriate for information that is missing or incompletely documented.
Avoid chart wars
- Do not joust in the record.
- Avoid criticizing other staff—current or former caregivers.
- Be aware that all relevant facts about prior care may not be available.
- Patient’s perceptions of care may be inaccurate.
- Conflicting chart entries undermine your credibility.
- Patient awareness of discordance may lead to loss of trust in caregivers.
- Use appropriate chain of command, not medical record, to address conflicts with other providers or administration.
- Do not prompt patients to consider litigation.
- Do not make assumptions; if something is not clear, get clarification.
- Do not amend or alter entries in the record without using the appropriate process.
Corrections/Addenda
- Paper: draw a line through incorrect entry with initials and the date. Provide corrected information.
- EHR: add a clearly marked addendum to the original entry with the corrected information; state the reason for the correction.
Do not delete or make original information inaccessible. - Do not make an addendum in anticipation of a claim or legal action because it may:
- be characterized as an attempt to falsify or change the record of fact
- appear to be “self-serving” rather than providing information that is needed for patient care
- seem defensive, may not contribute to the care of the patient, and should be avoided
Published in June of 2013, Revised January 2021
This page is an excerpt of a full issue of Insight.
CME: The Massachusetts Board of Registration in Medicine has endorsed each complete issue of Insights or 30-minutes of podcast episodes as suitable for 0.5 hours of Risk Management Category 1 Study in Massachusetts. You should keep track of these credits the same way you track your Category 2 credits.Recent Issues
Explore the archives.
Recently Asked Questions
Newsletter
Clinicians express concerns about malpractice and patient safety.


An Interest in What Went Wrong?
Newsletter
Why do the mistakes that enable patient injuries reoccur?

At the End of Information Blocking, an Opening for Patient Safety
Newsletter
Opening your notes offers the potential to enhance patient safety by linking clinicians and patients between visits-times when ambulatory vulnerabilities often compound.