Newsletter
MPL Risks Associated with NPs
Dec 31, 2019
Approximately 270,000 advanced practice registered nurses (NPs) were practicing in United States as of 2016,¹ with those numbers expected to grow by more than 30% over the next decade.² In almost all states, NPs now practice independently—with prescription privileges and, often, hospital admitting privileges.³ Concurrent with expanding their roles, NPs are increasing their medical professional liability (MPL) exposure.
To see if their expanded liability exposure has triggered an increase in medical malpractice allegations, CRICO conducted an analysis of 110,000 MPL cases from across the U.S. The Comparative Benchmarking system (CBS) database was queried for cases in which an NP was a named defendant. Both cases opened and cases closed from January 1, 2008 to December 31, 2018 were analyzed. Over those 11 years, fewer than 500 CBS cases involved an NP. Extrapolated to the entire U.S., that equates to about 150 MPL cases per year naming an NP.
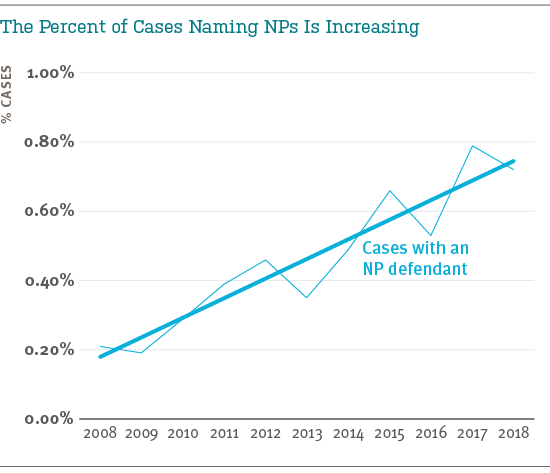
While the cases naming an NP represent a small portion of all MPL claims and suits, we do see an upward trend from 2008–2018. In 69% of their cases, NPs are named along with a co-defendant.
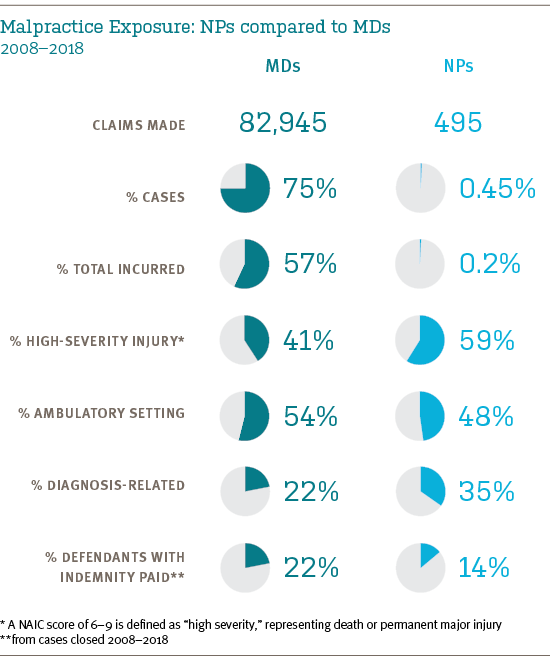
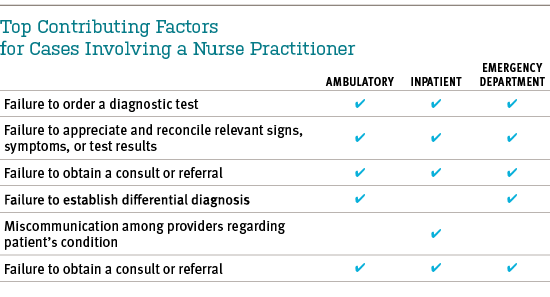
Nearly half of all NP cases involve (non-emergency) outpatient care. In that setting, their primary vulnerability involves diagnosis-related events leading to severe injury (or death): 43% of their ambulatory setting cases are diagnosis related, and 47% of those involve high-severity injuries. The key contributing factors seen in NP cases (across all care settings) are listed below.
In general, NPs are exposed to patient safety vulnerabilities similar to their physician colleagues. Organizations employing or insuring NPs can begin to identify opportunities to reduce exposure to situations that put patients—or other caregivers—at unnecessary risk, by considering the following questions.
- Is there clarity on scope of practice?
- Are accountable relationships based on unmodified state regulations, custom designed agreements, universal across all departments, or haphazard?
- Are there clear criteria for regular check-ins, escalation of care to a physician (e.g., patient factors or conditions that trigger MD involvement)?
- Are MDs and NPs educated about their malpractice liability, in particular regarding autonomous versus shared care?
- Do physicians within the organization believe NPs make them more vulnerable to malpractice allegations?
- Is the threshold for non-MD involvement in patient care extended indiscreetly?
- Are patients informed about the roles of NPs and their rights as patients?
- Is there team communication training in place?
Extending existing safety improvement programs to all members of patient care teams promotes a comprehensive understanding of risks, and greater likelihood that safety initiatives will be adopted and sustained.
References
A portion of the above content was previously published in the study Investigating MPL Vulnerability for the Institutions that Employ and Insure NPs and PAs, in the Aon/ASHRM Hospital and Physician Professional Liability Benchmark Analysis, October 2019 report.
- Bureau of Labor Statistics
- Kaiser Family Foundation State Health Facts: Physician Assistant Scope of Practice Laws
- AANP National Nurse Practitioner Database, 2019
Additional Material
Latest News from CRICO
A Comparative Analysis of Nurse Practitioner, Physician Associate, and Physician Malpractice Risk


Inform Safer Medical Oncology Practice with Lessons from Medical Malpractice Claims

An Analysis of Medical Malpractice Claims Against Medical Oncologists from a National Database: Implications for Safer Practice

