Newsletter
An In-depth Analysis of Medication-related Malpractice Cases
May 23, 2017

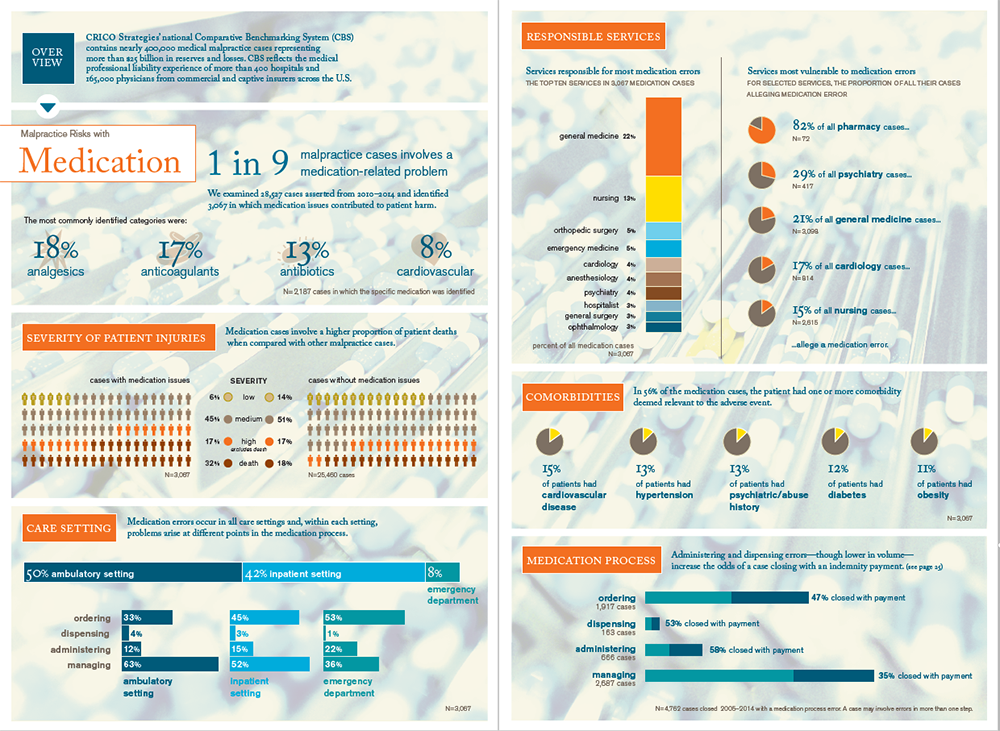
Despite significant strides in reducing errors in the mechanics of ordering, dispensing, and administering medications, one of every nine medical malpractice cases asserted from 2010–2014 involved an error in the medication process.
The bulk of those cases are triggered by events during the ordering and prescribing step (39%) and the monitoring/managing phase (56%). Breakdowns in patient assessment, clinical judgment, and communication are the most common issues; analgesics, anticoagulants, and antibiotics are the most common drug categories involved.
These findings are drawn from CRICO’s 2016 Candello Benchmarking Report: Medication-related Malpractice Risks. Univariate and multivariate analysis of 3,067 malpractice cases with an identified medication error shows that, when compared with non-medication events, medication-related malpractice cases:
- involve a larger percentage of deaths (32% v 18%),
- more frequently close with an indemnity payment (41% v 32%), and
- close with a considerably higher average payment ($453K v $354K).
Among the 3,067 medication cases, the key findings include:
- Primary care providers (22% of medication cases) and nurses (13%) are particularly impacted.
- Almost half of the drugs involved are analgesics (18%), anticoagulants (17%), or antibiotics (13%).
- Cases with dispensing or administering errors were most likely to close with a payment.
In many cases, a plaintiff alleging a medication error could point to unambiguous evidence: a documented allergy, a wrong drug selection, an inappropriate dose administered, a policy workaround. On the other hand, providers defending allegations of malpractice were challenged by the patient’s behavior: not taking medications as prescribed, unhealthy lifestyle choices, outright abuse. Between those extremes, the circumstances that led to an allegation of a negligent medication error were often as complicated as the patient’s health and the settings where he or she received care.
While hindsight may clarify the diagnostic and treatment challenges faced by multiple providers treating a patient who has multiple health issues, breakdowns in the medication process might, nevertheless, be perceived as avoidable. For more details on the most common types of medication errors, and what is being done around the country to reduce them, download the full Report.
Additional Material
Latest News from CRICO
Postpartum Malpractice Claims: Can We Understand Preventable Harms and Socioeconomic Factors?

The Safety of Inpatient Health Care

