Newsletter
What Is the Case About?
Feb 28, 2017
Every medical malpractice claim or lawsuit declares an error of commission or omission, but that moment is rarely where the case narrative begins or ends.
The scenarios that lead to assertions of substandard care often course through a range of factors, including the patient’s past medical history and the specific care the patient received (or should have) before or after the triggering event. Also to be considered, are the clinicians involved in that patient’s care and the systems they employ.
To determine the essence of what a given case is “about,” we have to fill in the background details of a complex, emotional, sometimes chaotic, and often temporally distant situation. That broader knowledge enables us to turn, for example, “this is a case about a technical error” into “this is a case about an OR nurse and anesthetist who were too intimidated to share key information that might have prevented an intraoperative complication.” The former description is informative, the latter is potentially actionable.
Understanding what a single case is “about” is even more actionable if you understand how frequently similar events occur. Reliable data about how many cases—in your state/organization/specialty/setting—involve retained foreign bodies during spinal surgery (or missed lung cancers related to incidental findings, misplaced gastronomy tubes, etc.) accelerates the motivation to explore deeper. Awareness initiates remedial (or even pre-emptive) action.
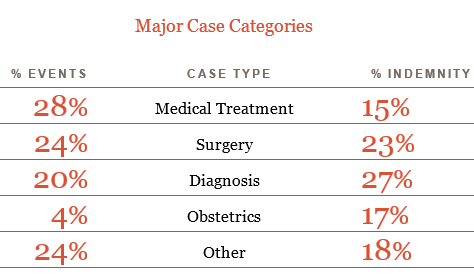
Analysis of 70,000 malpractice cases in CRICO’s national database stemming from events that occurred from 2004–2015, indicates that 77 percent of those cases allege an error in one of four categories: obstetrical care, surgery, medical treatment, and diagnosis. Cases from those same four categories account for 82 percent of dollar losses among cases closed with a payment from 2006–2015. Clearly, risk management and patient safety improvement resources need to target those four realms of health care.
Certainly, these are broad categories that represent the bulk of health care delivery. Awareness of more precise targets for risk management and patient safety improvement is gained through deeper mining and advanced analytics. The most vulnerable step in the diagnostic process, the riskiest labor and delivery decisions, common missteps in aligning provider and patient expectations during a surgery consent discussion, can be identified, even if you just begin with a single event and ask, what is this case about?
69,998 MPL cases with loss dates 2004–2015; $7.1B indemnity paid on cases closed 2006–2015.