Newsletter
A Sea Change in U.S. Care Delivery
Dec 18, 2023
“I think the main takeaway is that despite the dramatic increase in the number of APPs that are entering the workforce, the percentage of times they are involved in—or named as defendants—in these claims remains very low.”

Julie Higden
Senior Patient Safety Program Director at CRICO
A 13-year-old girl underwent a finger amputation following an incomplete telehealth evaluation for a finger abscess by a nurse practitioner. A claim was filed against the pediatric team for a delay in diagnosis and the case was settled. This case involved multiple providers and contributing factors relating to patient assessment, communication, and virtual care challenges. However, as the proportion of Advanced Practice Providers (APPs) in the workforce continues to grow, concerns have been raised that cases involving APPs might increase malpractice risk. So what do the data show?
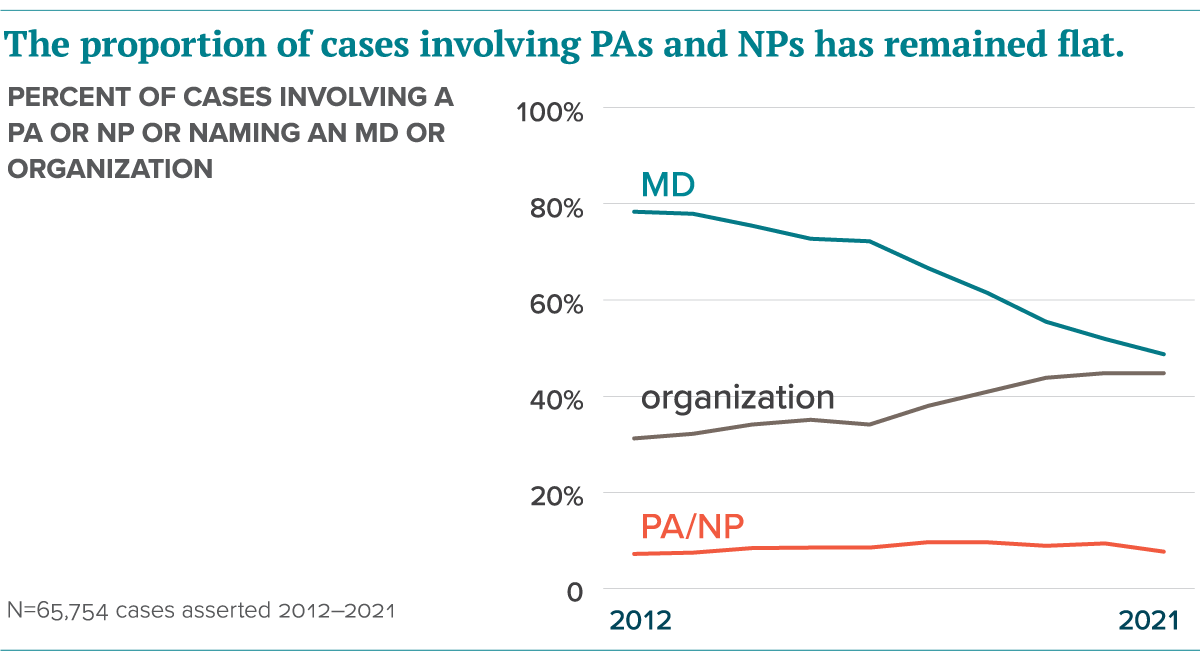
To help address these questions, Candello analyzed more than 65,000 malpractice cases asserted between 2012 to 2021 in their 2023 Annual Benchmarking Report. Findings showed Nurse Practitioners (NPs) and Physician Assistants (PAs) were rarely involved in the care or event that prompted a claim and were much less likely than physicians (MDs) to be named as defendants in medical professional liability (MPL) cases.
Julie Higden, a Senior Patient Safety Program Director at CRICO explains, “I think the main takeaway is that despite the dramatic increase in the number of APPs that are entering the workforce, the percentage of times they are involved in—or named as defendants—in these claims remains very low. We are also seeing that, despite the increase in the number of APPs in the workforce, the percentage of physicians named in these cases is also dropping quite dramatically, with about a 38 percent drop in physicians being named as defendants in these cases.”
Still, these APP cases offer valuable patient safety and risk management insights.
The analysts dove into the top contributing factors among cases and found patient assessment issues were involved in 43 percent of cases. As shown in the table below, cases with patient assessment issues had higher odds of closing with payment compared to cases without this contributing factor. As patient assessment issues are commonly seen across claims regardless of the clinical training of the individuals involved in the care in question, the contributing authors provide recommendations to address assessment challenges.
- Uphold best practices when documenting complete patient history
- Conduct thorough physical exams to establish differential diagnoses
- Enact protocols for providers to reconcile relevant signs, symptoms, test results, and receive complete information from diagnostic tests in a timely manner
- Use safety net systems to ensure proper follow-up on test results and incidental findings
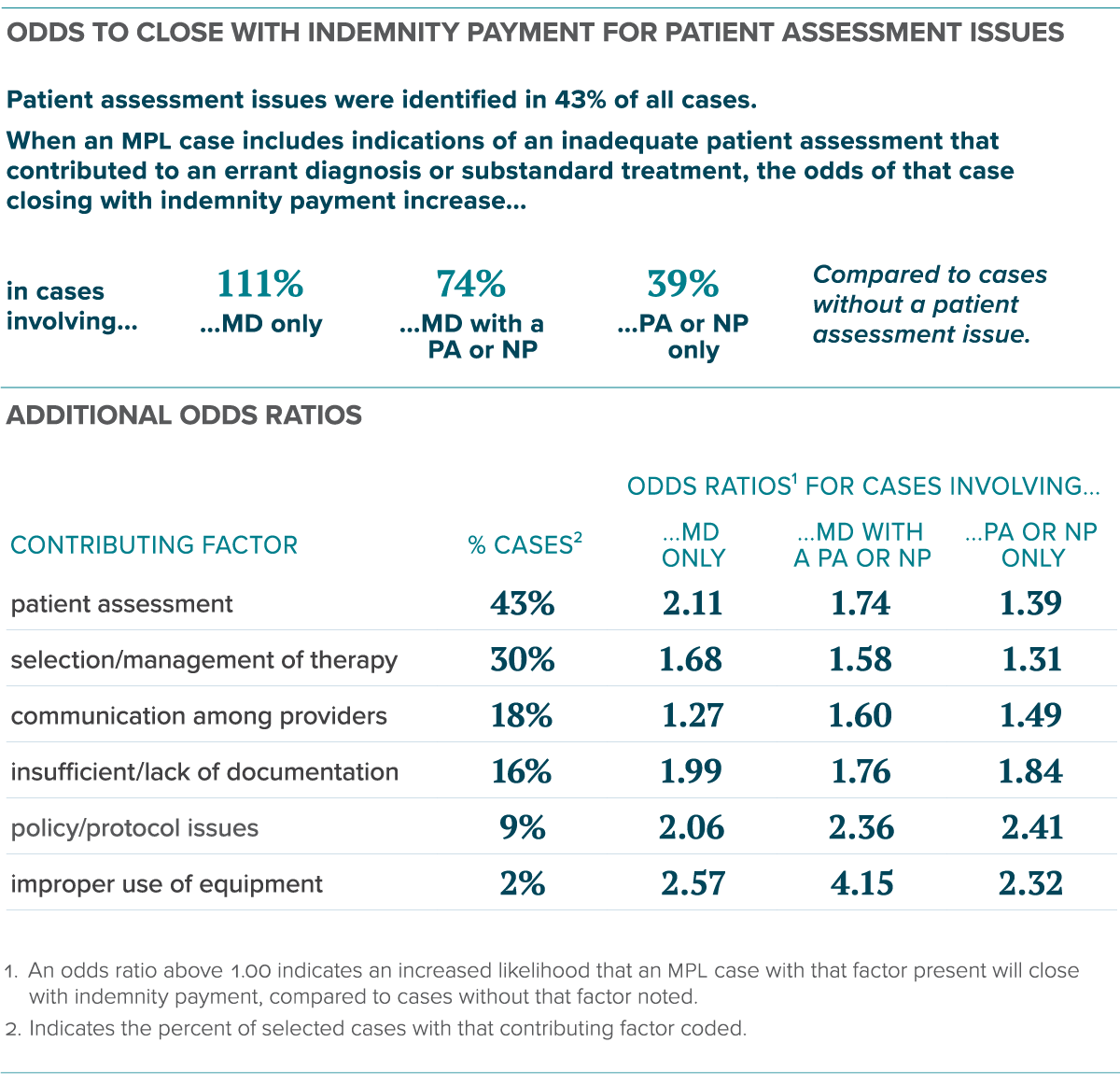
Cases involving an APP did present greater financial risk with 41 percent of PA cases closing with pay, 40 percent of NP cases closing with pay, and 36 percent of MD cases closing with pay. Cases involving physicians also had significantly lower closed-with-pay rates than those involving an APP.
The report stresses the necessity of organizational leaders implementing processes to successfully integrate APPs into the provider workforce to increase engagement, retention, and promote effective team communication to enhance patient safety. Considerations surrounding APPs continue as rules and regulations change for the scope of practice, especially as APPs fill gaps in primary care to increase health services access across the population. It will be imperative to track these trends over time, but for now, be assured that there has not been an observed increase in the proportion of MPL claims involving nurse practitioners or physician assistants.
Additional Material
- Free Download: Candello 2023 Benchmarking Report: A Sea Change in U.S. Care Delivery: An Analysis of Advanced Practice Provider and Physician Malpractice Risk
- Podcast: Higher Malpractice Risk with Advanced Practice Providers? The Data Say Not Really
- Where Can Nurse Practitioners Work Without Physician Supervision?
- In What States Can Physician Assistants Practice Independently?
Recent Issues
No Surgical Items Left Behind


Top Contributing Factors to Medical Malpractice Claims Deliver Clarity to Sources of Medical Error

Why Went Wrong

