Newsletter
Who’s Running the Code? Improving Communication in Health Care
Nov 29, 2023
Miscommunication, particularly among providers, continues to be a top contributing factor in medical malpractice claims across clinical disciplines. In their 2022 review, The Joint Commission named failures in communication and teamwork two of the leading causes of sentinel events, i.e., patient safety incidents that result in death, permanent harm, or severe temporary harm.
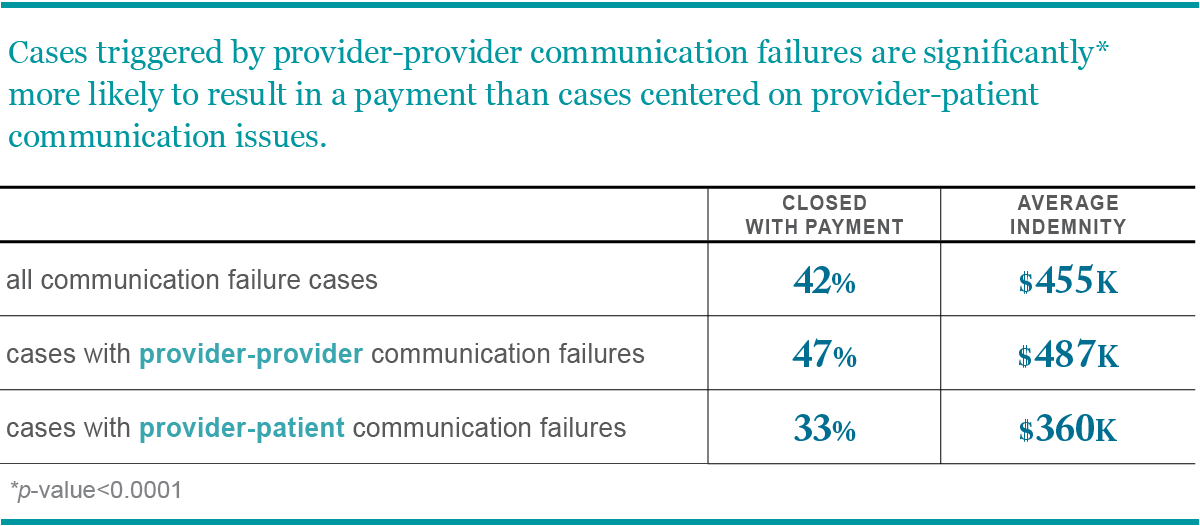
In terms of malpractice claims, Candello released a benchmarking report in 2015 that examined more than 7,000 cases listing communication failure as a contributing factor. The analysis highlighted that malpractice cases involving provider-provider communication failures are significantly more likely to result in a payment when compared to cases featuring provider-patient miscommunication.
In recent years, simulation-based team trainings have gained more traction as an effective way to bolster provider communication and lower risk. As dress rehearsals are essential for a theater cast and crew to fix their mistakes without an audience, medical simulation gives clinical teams the chance to address communication breakdowns and process failures without jeopardizing patient safety.
Simulations for medical training date back centuries, and as they have evolved with technology, health care simulation technology assumes a pivotal role as a sophisticated training platform, meticulously designed to replicate the intricacies of authentic clinical challenges. Simulations also became vital during the COVID-19 pandemic, allowing administrators and providers to test protocols and standardized communication to protect both provider and patient safety.
The obstetrics and gynecology field has specifically embraced immersive, simulation-based trainings as OB/Gyns are more likely to be named in a malpractice case than the national average for all physicians. A study led by Adam Schaffer, MD assessed malpractice claim rates among 292 obstetrician-gynecologists who attended one or more high-acuity simulation trainings between 2002 and 2019. Scenarios included a full-term pregnant patient with a traumatic injury during labor and acute postpartum maternal compromise requiring life-saving intervention.
Throughout the study period, malpractice claim rates (per 100 physician coverage years) were significantly lower following simulation training. Attending more than one simulation was also associated with a lower claim rate, and attending three or more simulations was associated with the lowest claim rate.
Team training simulation has often been used to allow teams to work together on high-acuity, infrequent events, such as cardiac arrests. However, mock health care scenarios and role play are not just for emergency situations. I-PASS, an award-winning methodology working to standardize the handoff process, uses virtual, simulated handoff experiences as one of its components to help reduce the risk of medical error during patient handoff.
Regardless of the scenario, these lifelike situations give clinicians the rehearsal space to identify and rectify mistakes, ultimately improving provider communication behaviors, lowering liability risk, and protecting patient safety.
Additional Material
- Joint Commission Sentinel Event Data 2022 Annual Review
- The Center for Medical Simulation
- Malpractice Risks in Communication Failures: Candello’s 2015 Annual Benchmarking Report
- I-PASS Patient Safety Institute
- Just-in-Time In Situ Simulation Training as a Preparedness Measure for the Perioperative Care of COVID-19 Patients
- Association of Simulation Training With Rates of Medical Malpractice Claims Among Obstetrician-Gynecologists
- Simulation Fit in Healthcare
Recent Issues
Enhancing Mentorship in Medicine with Malpractice Data


Patient Safety Playlist


