Newsletter
From Click to Care: Managing Copy-and-Paste Risks in the EHR
May 31, 2024
In the realm of word processing, the convenience of copy and paste is undeniable. But what risks does this shortcut present within the electronic health record (EHR)? In this edition of Strategies for Patient Safety, we delve into the complexities surrounding copy-and-paste errors, examining real cases and offering practical recommendations to safeguard patient well-being while navigating potential medicolegal risks.
While the shift from paper to digital records has revolutionized health care delivery, documentation remains a significant time investment for physicians. A 2018 Annals of Internal Medicine study revealed physicians dedicate approximately 44 percent of their time to documentation on the computer, with a mere 24 percent spent on direct patient interaction.
To grasp the extent of risk posed by copy-and-paste and other EHR user errors in clinical practice, Candello conducted a thorough analysis of cases closed between 2017 and 2021. As depicted below, EHR-related issues comprised roughly one percent of cases, with about one-third of those cases involving pre-populated or copy-and-paste elements. This relatively small number of clinically coded cases still provides meaningful insights into malpractice risk in documentation, which remains one of the largest contributors to medical errors and injury in the U.S.
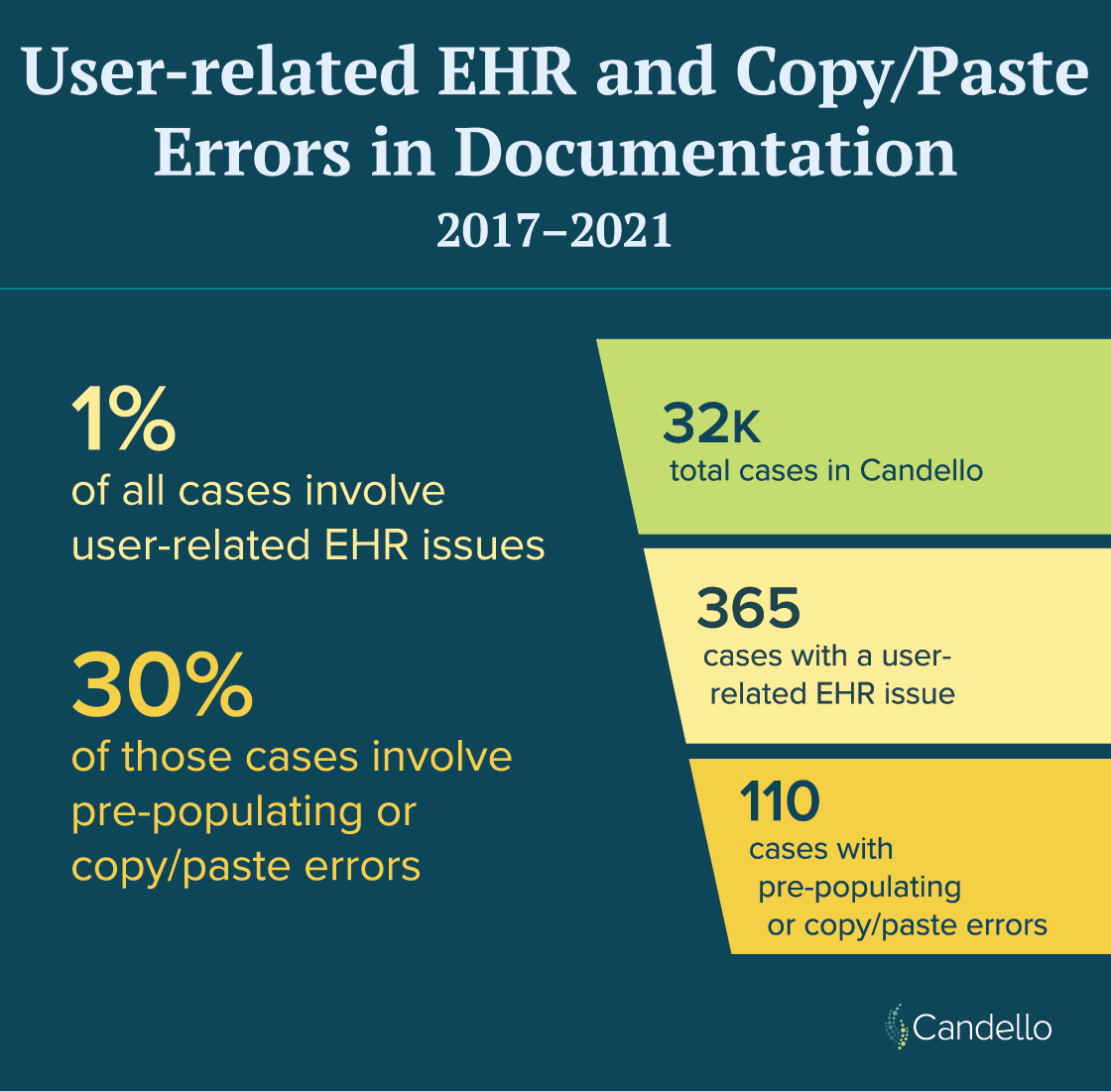
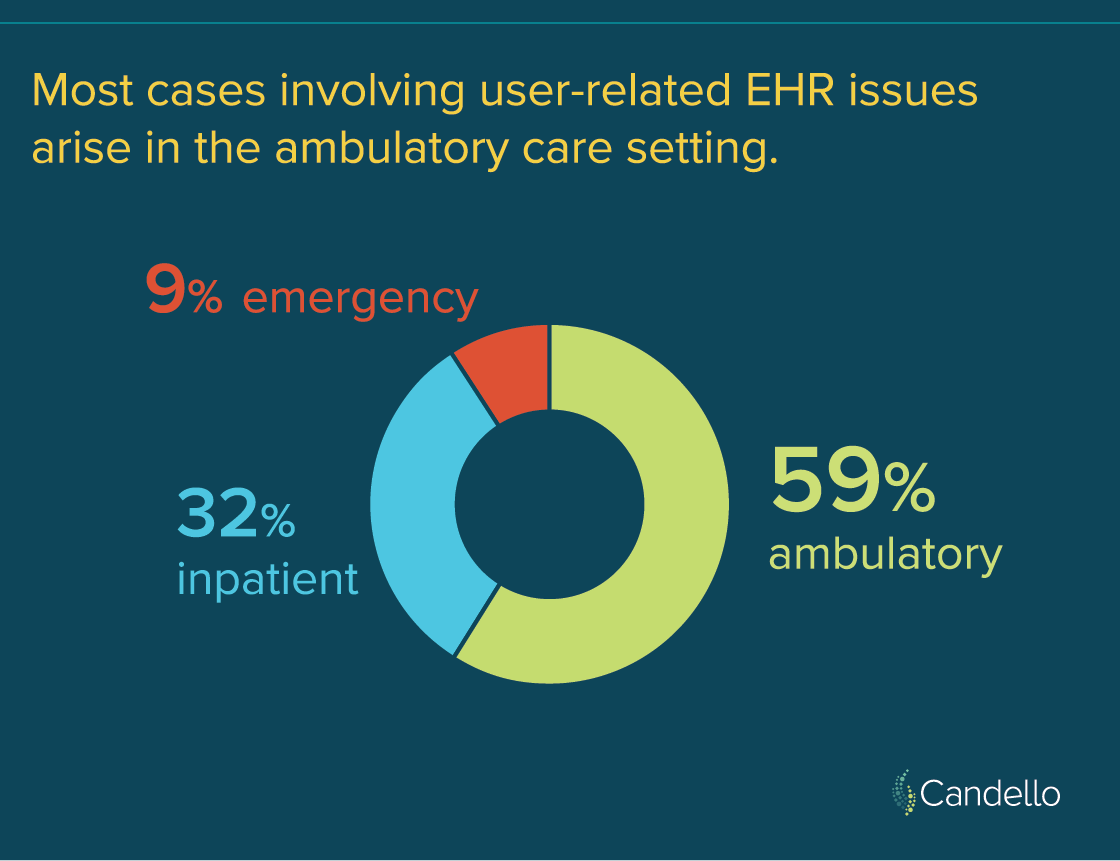
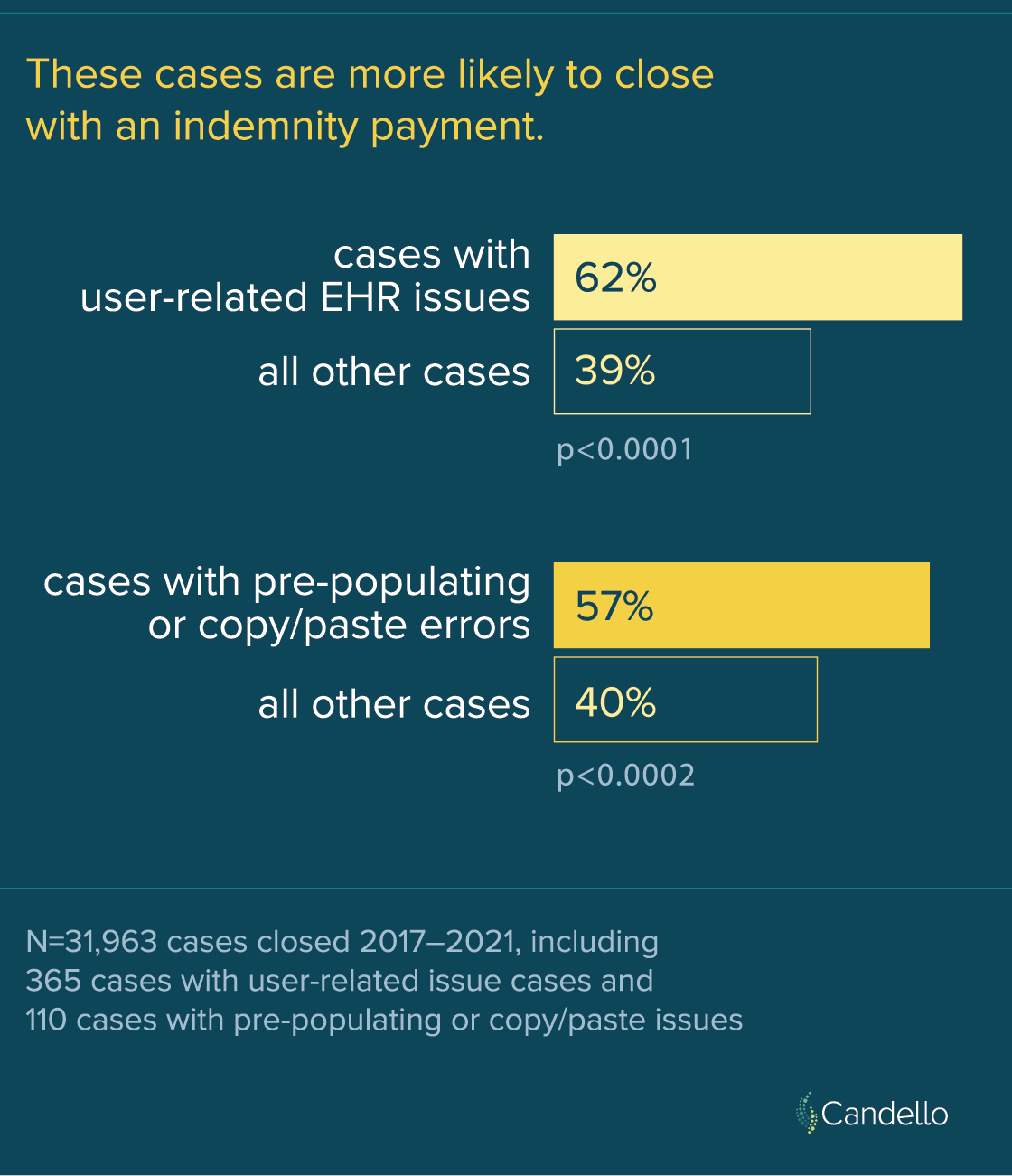
These EHR-related challenges encompassed user errors, training deficiencies, and inaccuracies within records. While infrequent, both EHR-related and copy-and-paste cases demonstrated a higher likelihood of closure with payment compared to other Candello cases. However, the average indemnity payment for EHR-related and copy-and-paste errors hovered around $450K and did not significantly differ from the average payment for the other cases in the database.
So, what measures can be taken to ensure that patients’ medical records bolster appropriate care and safeguard providers amidst potential malpractice claims?
At the organizational level, health care institutions can ensure their EHR system has a feature that clearly indicates copied text and its date of origin. Monitoring and implementing policies and training programs regarding the copy-and-paste functionality can also be effectives steps.
On an individual level, providers can enhance documentation practices by verifying notes and avoiding the use of specialty-specific abbreviations that may cause confusion. Structuring notes into distinct sections, such as active issues, resolved issues, and compliance-related text facilitates clarity for other providers caring for the patient.
“We should try to avoid ‘note bloat’ in which our notes contain resolved clinical issues or extraneous text that may make it difficult for colleagues who read our notes to focus on the patient’s active issues,” says Adam Schaffer, MD, MPH, hospitalist at Brigham and Women’s Hospital and Senior Clinical Analytics Specialist at CRICO. “One big risk with using copy/paste in our notes is copy-and-paste clinical reasoning, in which one assumes a certain symptom is due to a condition the patient already has and does not consider the possibility of a new diagnosis. This resembles the cognitive error of premature closure and is a setup for misdiagnoses.”
Documentation serves as a linchpin for continuity of care, inter-provider communication, compliance and billing, and it often stands as the cornerstone of evidence in medical malpractice cases.
For further insights into mitigating copy-and-paste risks and fostering robust documentation practices, consider enrolling in CRICO’s free CME course. This activity is also designed to be suitable for one hour of Risk Management study in Massachusetts.
Recent Issues
Test Ordering Risks and Remedies


Recently Asked Questions

