Podcast
Teleradiology Leads Virtual Care Risk in New Study
Oct 24, 2024
“Our study pointed to a potential risk with over-reading, which is, if no one knows to look out for this second read, then any findings arising from this second read that requires a response may not be acted upon.”
Adam Schaffer, MD, MPH
Senior Clinical Analytics Specialist, CRICO
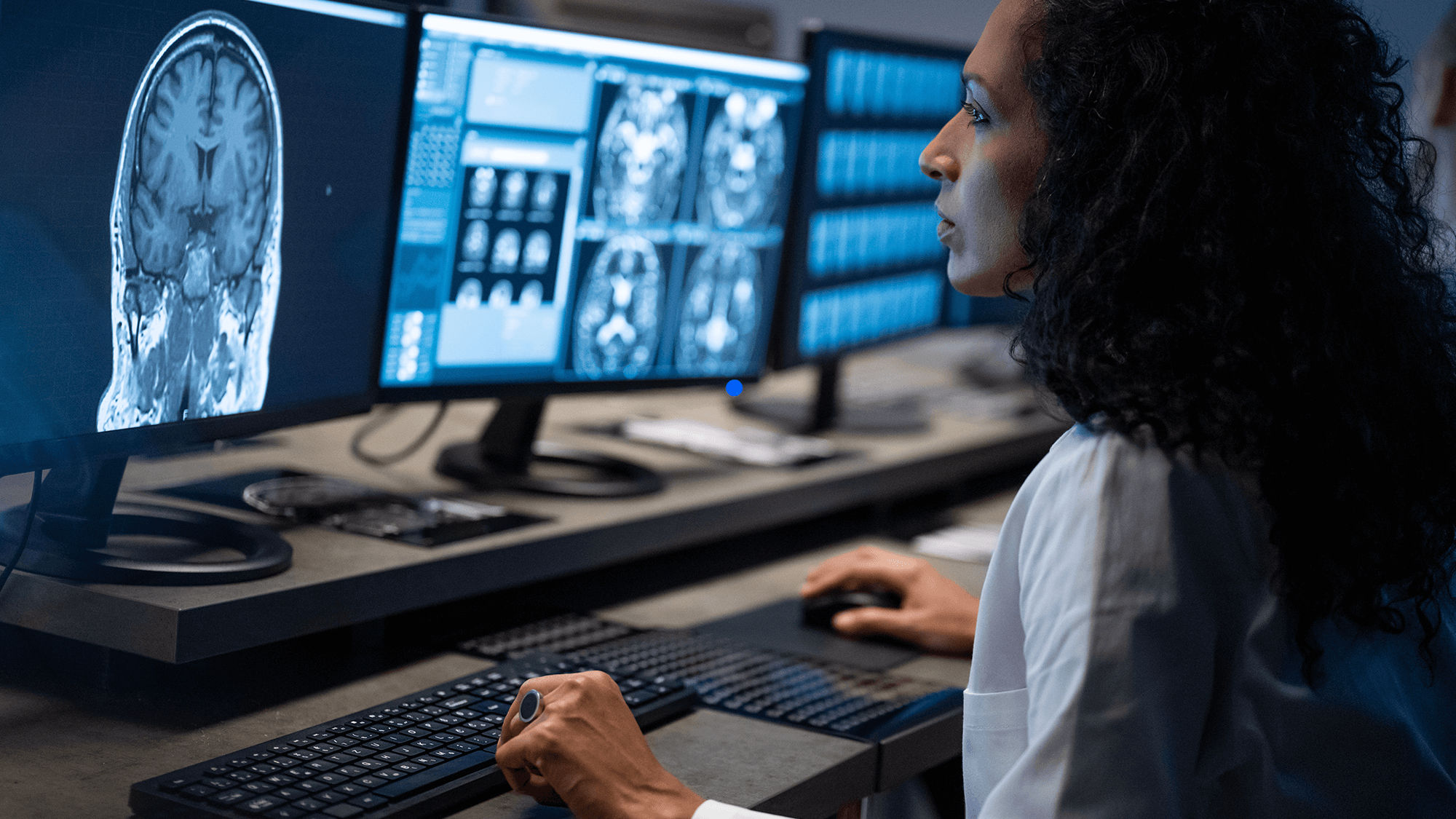
New original research in the journal Radiology reveals a stark difference comparing teleradiology cases and radiology cases without a telemedicine factor. A review of more than 3,600 medical professional liability cases in a national database over a recent 12-year period showed higher clinical and financial severity for teleradiology services compared to other radiology cases in general. But this discovery wasn’t the malpractice researchers’ original focus.
“The genesis of this project was an interest in telemedicine more generally in the setting of the COVID pandemic.”
Dr. Adam Schaffer is a hospitalist at Brigham and Women’s Hospital and Senior Clinical Analytics Specialist for CRICO. He is also the lead author of the study.
“When COVID hit, there was a sudden and dramatic increase in one type of telemedicine, which is virtual visits. With the increase in virtual visits, we decided to examine our telemedicine claims as part of examining the risks we might expect to see with virtual visits.”
The data come from the Candello database of more than 475,000 medical professional liability claims from hundreds of healthcare entities, representing a third of all med-mal claims in the United States. The researchers first found that the highest telemedicine risk wasn’t a virtual office visit at all. Rather it was teleradiology—the remote interpretation of images—that was blinking yellow.
“Somewhat to our surprise, we found very few cases related to virtual visits, which provides a degree of reassurance when it comes to the liability risk associated with virtual visits. However, we found that the most common type of telemedicine case was actually teleradiology. Of the 223 telemedicine cases we identified in our Candello database, roughly 60% of them were teleradiology cases. This prompted us to look deeper into these teleradiology cases to try to better understand some of the underlying patient safety and medicolegal issues.”
In Dr. Schaeffer’s study, teleradiology malpractice cases were compared with radiology cases without a telemedicine component. Among the key risks that appeared in the data were that teleradiology cases were more than twice as likely as radiology to involve communication among providers as contributing factors. These cases were far more likely to result in death, and the teleradiology cases also closed with higher average indemnity payment.
One counterintuitive finding was a high risk with over-reads, which are designed to provide more safety with a second set of eyes. But it doesn’t surprise one of the study co-authors. Dr. Aaron Sodickson is an Associate Professor of Radiology at Harvard Medical School, and Medical Director of Enterprise Radiology for the Mass General Brigham network. Dr. Sodickson points out that the nature of teleradiology is that initial overnight reads are done remote to the patient and are often done as a preliminary read. The next day the radiology practice at the home institution local to the patient reviews it again and makes a final report.
“And in many ways, that’s good for patient safety. You have two sets of eyes with qualified radiologists reading the studies, but there are a couple of challenges that it raises. One, it more directly draws attention to discrepancies, because you have now an initial read and a final read that, you know, would demonstrate differences in interpretation. So that might be why there is some increased teleradiology risk even if we think it is better for patient care.”
More than the legal risk of a discrepancy sitting in the patient’s chart, is what can happen to the patient if the discrepancy is not addressed in a timely way. Dr. Sodickson says the mistake made by some of the home institutions receiving an overnight teleradiology read is to think it’s not a priority since it’s been read once already.
“The other possibility is that if the final read is not done very promptly, then you now have a delay in which harm can come to the patient. So if there is a missed diagnosis that is time critical, as is sometimes the case for these ED or ICU patients, that time delay really matters, and so rather than getting a final read out there immediately or getting a perfectly accurate initial read done by teleradiology, we now have a delay before a critical diagnosis is found, which I think could increase risk.”
The systems and protocols that surround these teleradiology over-reads can make or break an individual result. Dr. Sodickson says reaching the patient or the ordering clinician can be further challenged when patients transfer out of the home institution or the first doctor is no longer on duty.
Dr. Schaffer:
“Our study pointed to a potential risk with overreading, which is, if no one knows to look out for this second read, then any findings arising from this second read that requires a response may not be acted upon. To provide a very concrete example, let’s say the patient presents on a Saturday night to the emergency department with shortness of breath. The ED doctor orders a special chest CT looking for a blood clot in the lungs, known as a PE CT. This CT is read by a teleradiologist, who identifies no blood clot, no pneumonia, or other urgent findings, and so the patient, who is now feeling better, is discharged from the emergency department. The hospital radiologist comes in Monday morning, and then overreads this chest CT. She agrees that there is no blood clot or other urgent finding. However, she notices a small lung nodule that is indeterminate, and so recommends following up in 6 months to make sure it is not growing, as a growing lung nodule would be concerning for possibly being a cancer and so you’d want to do additional diagnostic workup. This overreading report is generated in the electronic medical record.
However, the emergency medicine physician who saw the patient is likely to longer working a shift in the ED, and may not even know that the overreading was going to occur, since a radiology report was already generated and finalized by the teleradiologist. And the patient has been discharged from the ED. So, under circumstances such as this, and variations of which we saw in the teleradiology malpractices cases, there is a risk that new actionable findings arising from an overread may be missed.”
Dr. Schaffer says it is important to give teleradiologists the context for the order, and access to the patient’s relevant records whenever possible. The clinician who orders the teleradiology study needs to be informed that there will be a subsequent read. And the over-reading radiologist should reach out to the ordering clinician with any new, actionable findings.
“A key principle of patient safety is that you do not want to rely exclusively on the vigilance of individuals to avoid adverse events, and you want to try to build redundant systems that supplement the efforts of individual providers. Tests pending at discharge refer to tests for which final results are not available at the time the patient is discharged from the hospital. Tests pending at discharge include things such as blood cultures that may grow bacteria after the patient has left the hospital. There are systems in place for tests pending at discharge—including closed loop notification systems and clinicians who are specifically tasked with responding to follow up on these tests. I think we should consider ways we can apply these existing systems designed to handle tests pending at discharge to overreading results.”
Dr. Sodickson says extra attention is needed from the ordering and the receiving institutions and providers, as to what happens to teleradiology results, if we are to lessen risks for a technique designed to lessen imaging delays. He says a current shortage of radiology personnel is raising the stakes for everyone.
“It’s worth pointing out that most practices simply don’t have the scale to provide 24/7 coverage of all of their imaging needs internally. And so over the years teleradiology has really been tremendously helpful in closing some of those coverage gaps and enabling contemporaneous interpretations for things that, in the old days might have waited many hours to be read the next morning… I think it really comes down to setting institutional procedures and expectations, making sure that there is clarity on who should receive these calls and who has the responsibility to act on them. I think that’s something that’s challenging to do, particularly with these teleradiology practices that might be dealing with multiple different hospitals out there.”
I’m Tom Augello, for Safety Net.
Commentators
- Adam Schaffer, MD
- Aaron Sodickson, MD, PhD
About the Series
We’ve got you.
Our Safety Net podcast features clinical and patient safety leaders from Harvard and around the world, bringing you the knowledge you need for safer patient care.
Episodes
How Application Forms and Burnout Threaten MD Mental Health and Patient Safety
$1.5 Billion in Miscommunication: Medmal Data Report Finds Opportunities

Case Dismissed! Every Medical Defendant’s Dream Still Holds Some Nightmares

Expert: Communication Is Top Fix for Prostate Care Allegations