Newsletter
Managing Non-coronavirus Patients’ Expectations Amid the Pandemic
Mar 27, 2020
In recognition of the unique commitment of health care workers during the COVID-19 pandemic, we hope to witness deep appreciation and patience across the communities dependent on them. Unfortunately, even among patients whose health care concern is unrelated to the crisis, civility may erode under duress and uncertainty. Everyone’s tolerance is being tested.
While the pandemic dominates our news cycles and workdays, patients with a pressing non-COVID-19 health concern may worry that their needs won’t or cannot, be met. Below are a few suggestions to help guide expectations for anxious patients and family members during this crisis.
Familiarize yourself with your organization’s messaging to patients.
Clinicians and staff should read the broadly distributed messaging (emails, website, social media, phone recordings) regarding the impact of COVID-19 on appointments, prescription renewals, virtual visits, emergency care, etc. Seeing and hearing the information your patients are receiving helps reduce confusion or mixed messaging.
Respond to patients as quickly as possible.
Clinicians in all settings are likely to have fewer (non-COVID-19 related) appointments/procedures during periods of restrictions aimed at minimizing its transmission. Concurrently, patients with acute care concerns may need extra reassurance that their questions and concerns are being heard—that you’re there when they need you. Individuals frustrated by a lack of response via emails and patient portals may subsequently tie up your phones. Consider how colleagues who may be less busy due to cancellations of elective care could step in to answer patient queries.
Encourage sick or injured patients to seek care and continue treatment.
Non-COVID-19 patients may forgo appointments or care out of fear of exposure, or as an altruistic effort to free up caregivers, putting those with serious health issues at greater risk. Where possible, help all of your patients understand that, while the appropriate threshold for seeking care may change during this crisis, anyone who is sick or injured should still seek care or, at least, check in with a telephone or online triage resource.
Balance communication preferences with confidentiality and liability concerns.
While many organizations are suspending or altering restrictions on the use of non-secure communication modes, care and caution remain important. Clearly identify the person on the other end of any exchange and document care and decision-related discussions (oral or written) that are not automatically posted to the patient’s record. If documentation (e.g., informed consent) is complicated by the avoidance of face-to-face contact and document exchange, consider including a third-party witness.
Virtual visits require planning and caution.
As many providers and patients clamor for a robust virtual visit environment, the potential impact on medical professional liability cannot be waived away. Most major health care organizations have some experience moderating telemedicine and other forms of non-face-to-face patient care, but such practice may be brand new to smaller organizations and individual clinicians. Document virtual visits like a live encounter and be cognizant of the inherent limits of such technology, such as the inability to perform a physical exam.
Helping patients understand how their situation will be managed within an upended and overtaxed health care environment is key to aligning their expectations with yours.
Additional Health Care Provider Liability and COVID-19 Material
Latest News from CRICO
Characterizing Malpractice Cases Involving Emergency Department Advanced Practice Providers, Physicians in Training, and Attending Physicians

Utilization of Electronic Health Record Sex and Gender Demographic Fields: A Metadata and Mixed Methods Analysis

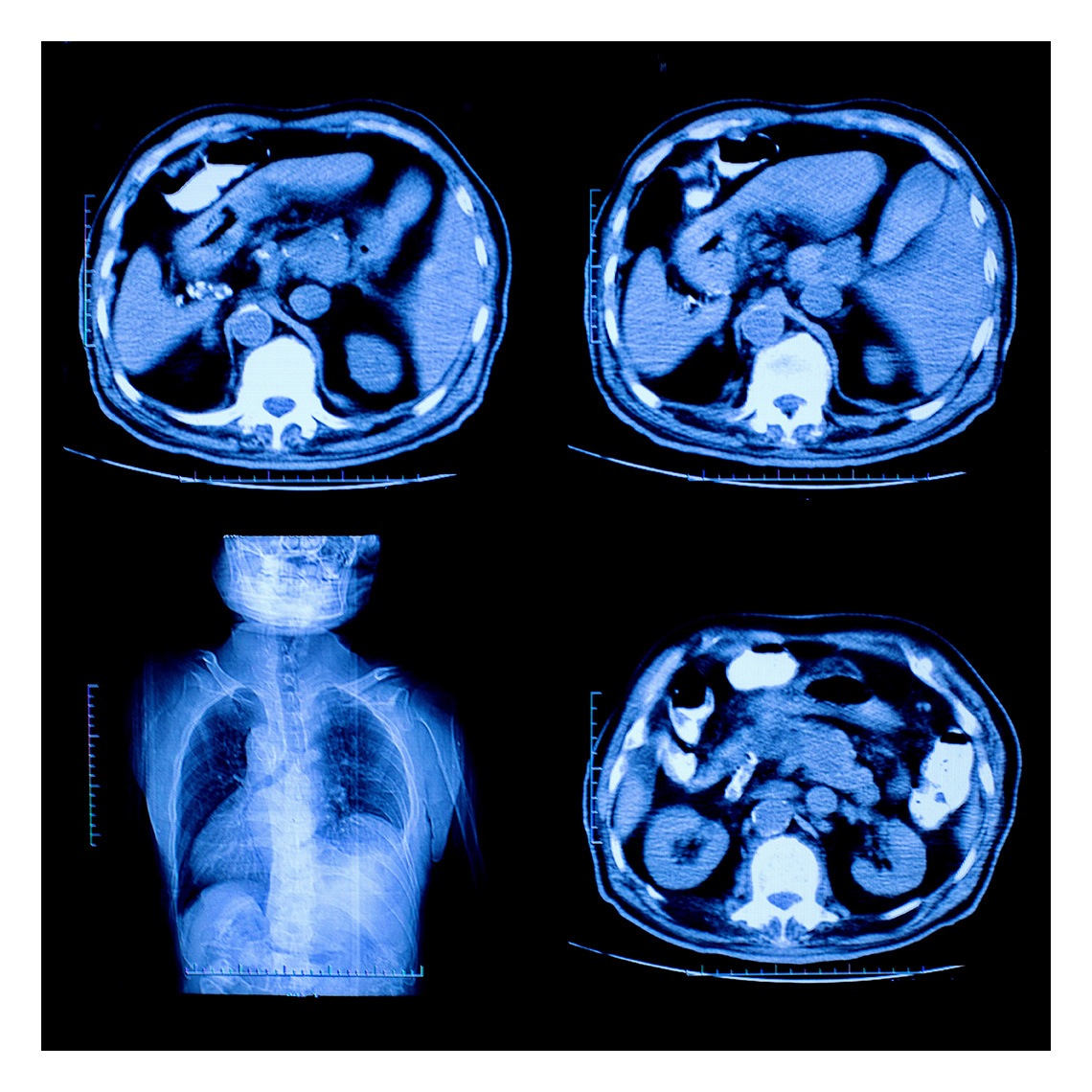
Teleradiology Medical Malpractice Cases