Newsletter
For the Record: Key Documentation Lessons to Take Into 2025
Dec 19, 2024
For the Record: Key Documentation Lessons to Take Into 2025
As we look forward to the new year, we reflect on the invaluable insight provided by the 2024 Candello Benchmarking Report—a comprehensive analysis that has sparked important conversations about the role of documentation in patient safety and malpractice risk. Over the past month, we’ve explored the data, highlighted critical risks, and shared actionable strategies. Now, in this final article of the year, we revisit the key takeaways and reflect on how healthcare leaders can use this knowledge to improve care and fortify defensibility in the year ahead.
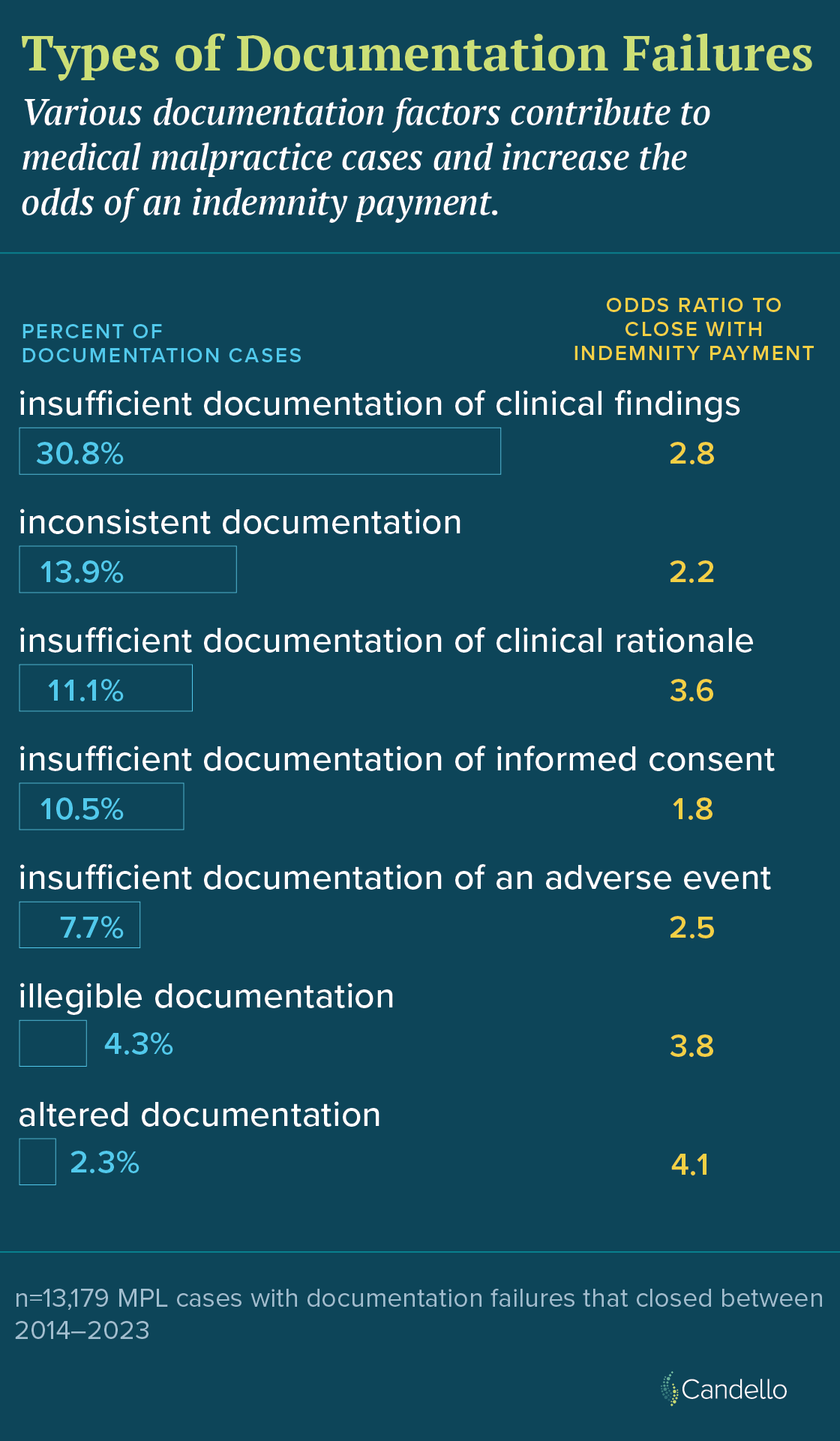
During the past decade, documentation failures played a part in 20 percent of closed medical professional liability (MPL) cases each year on average. Problems with the medical record led to 140 percent higher odds of case payout compared to cases without documentation issues. Furthermore, cases with documentation factor(s) involved greater clinical severity, with 50 percent involving high-severity injuries or death compared to 41 percent for cases without documentation issues.
The report describes how some documentation errors are more costly than others.
Specialties at Higher Risk
Every clinical service included in the analysis saw higher odds of closing with payment when documentation was a factor. However, certain specialties, such as surgery, obstetrics/gynecology (OB/Gyn), anesthesiology, emergency medicine, and nursing were particularly prone to documentation-related malpractice risks:
- Surgery: Cases involving documentation issues were more likely to close with payment (53 percent vs. 31 percent), often due to lapses in informed consent or incomplete operative notes.
- OB/Gyn: These cases incurred the highest average indemnity payments when documentation errors were involved ($820K vs. $670K).
- Anesthesiology: Anesthesiology cases with documentation failures were nearly twice as likely to involve high-severity patient injuries (55 percent) compared to those without documentation issues (31 percent).
- Emergency Medicine: Fast-paced environments contributed to missed or delayed documentation of diagnostic tests and follow-ups, contributing to higher payouts and clinical severity.
- Nursing: Thirty percent of all nursing cases involved a documentation issue, with the documentation of adverse events and undocumented clinical findings being some of the more common errors.
The Role of Technology
While electronic health records (EHRs) and artificial intelligence (AI) tools have streamlined clinical documentation, they also introduce significant risks that require careful management and the clerical burden on physicians is still ever present. Copy-paste practices can lead to "note bloat," burying critical details and increasing the risk of documentation errors. Patient portals enhance transparency but necessitate precise, patient-friendly language to avoid misunderstandings or disputes. AI tools, though promising, require rigorous oversight to mitigate risks such as bias, inaccuracies, and data quality issues.
Actionable Recommendations
The report offers several best practices to mitigate documentation-related risks:
- Document Clinical Rationale: Clearly articulate reasoning behind diagnoses and treatment decisions.
- Address Adverse Events Promptly: Follow organizational guidelines to factually and promptly document incidents.
- Avoid Inconsistent Entries: Ensure seamless communication and alignment across all providers.
- Enhance Informed Consent Processes: Record comprehensive discussions of risks, benefits, and alternatives.
- Minimize Copy-Paste Usage: Include only relevant, current information in notes.
- Capture Non-Adherence: Record instances of patient non-compliance and associated follow-up instructions.
- Foster Inclusive and Respectful Language: Avoid stigmatizing or prejudicial comments that could undermine legal defensibility.
Closing the Gap in Defensibility
Strong documentation practices not only improve patient care but also fortify a provider’s ability to defend their care in malpractice cases. The report emphasizes that even in adverse outcomes, clear and comprehensive records of clinical decisions can enhance credibility and support favorable resolutions. In cases involving disputes, accurate documentation can be the decisive factor in determining legal outcomes.
As we move into the new year, these findings serve as both a call to action and a guide for fostering a culture of precision, accountability, and safety in health care. Let this year-end reflection not be a conclusion, but a springboard for continued progress in 2025 and beyond.
To uncover more lessons detailed in “For the Record: The Effect of Documentation on Defensibility and Patient Safety,” request your copy now.
Additional Resources
A Physician’s Perspective: If You Don’t Document It, It Didn’t Happen
Continuing Medical Education: Documentation Risks in Malpractice Cases: Copy & Paste Risks
AMA Article: 7 EHR usability, safety challenges—and how to overcome them | American Medical Association
Recent Issues
From Click to Care: Managing Copy-and-Paste Risks in the EHR


When Protection Creates Risk: Licensing Reform and Mental Health Stigma in Health Care

Raising the Bar for Risk Assessment

