Article
Risks in Radiology: Contributing Factors
What’s My Risk?
Contributing Factors in Medical Malpractice Claims against Radiologists: How to Protect Your Patients and Yourself
Deep analysis of more than a decade of medical professional liability (MPL) cases reveals that those involving radiologists are most commonly related to missed or delayed diagnoses, in particular, cancer, fractures, and post-procedure complications. While radiologists are most vulnerable to allegations of having misinterpreted a screening or diagnostic image, they are also at risk for failing to adequately communicate their findings to the ordering provider (and, in some cases, patients). Thus, while a primary care provider may have carried out the bulk of a patient’s diagnostic process, missed or delayed diagnosis allegations are often filed against the radiologist.
As a radiologist, your goal is to deliver the highest-quality care for your patients. Yet in the fast-paced world of a complex health care system, things sometimes don’t go as planned. When oversights or errors occur, either the course of the patient’s diagnosis or the efficacy of treatment may be compromised, and you may be named in a medical malpractice claim or lawsuit. In fact, radiologists are more likely to be named in a malpractice case than the national average for all physicians1. Further, in half of all medical malpractice claims that name a Radiologist, the patient suffered a permanent serious injury, or died.
To help mitigate associated risks with this specialty, CRICO conducts detailed analyses of its national MPL database and works with departmental and organization leaders to help radiologists understand their patient safety vulnerabilities and support opportunities to improve systems and training related to those risks.
Identify Key Vulnerabilities
Whether you are insured by CRICO or another MPL underwriter, you can protect yourself—and ensure the best outcomes for all involved—by taking the time to understand the most common risks seen in cases against Radiologists. Candello’s national Comparative Benchmarking System captures 30 percent of all medical professional liability cases across the U.S., providing a wealth of data that can help you identify your specific areas of malpractice risk. Using that same data, CRICO has also developed risk mitigation resources intended to offer radiologists concrete opportunities to improve their safety profiles.
A unique and highly-detailed component of the Candello data is capture of the clinical and practice environment issues that had a direct impact on the events that triggered allegations of malpractice. Knowing and exploring those contributing factors offers direct guidance for reducing the risk of patient harm and best practices for avoiding, or defending, an allegation of substandard care.
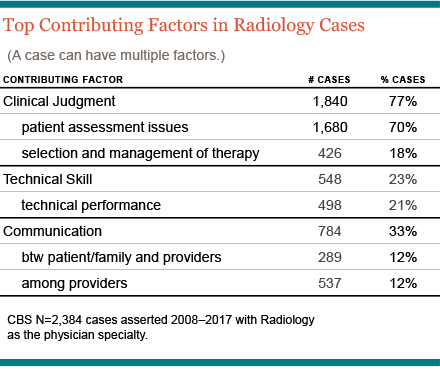
Learn More About the Top Three Contributing Factors in Cases Naming Radiologists
Compared to physicians in many clinical specialties, radiologists generally have a less established relationship with their patients. They are primarily communicating with peers and the ordering physicians and, typically, are disengaged from the patient’s subsequent course of care. For radiologists, allegations of medical malpractice are almost exclusively focused on issues related to image interpretation, results communication, and follow-up recommendations. The top three contributing factors in cases naming radiologists are:
- Inadequate Patient Assessment: For radiologists, 4 out of 5 cases involve one or more patient assessment issue. These are primarily allegations of misinterpretation—based on subsequent imaging and reads by clinical experts who are retrospectively able to identify anomalies related to the patient’s eventual diagnosis. Radiology cases may also point to a failure to appreciate the relevance of the patient’s results, or to order follow-up imagings.
- Miscommunication: One-third of cases reflect a breakdown in communication among providers between the radiologists and the patient, almost always about test results or the subsequent care plan. While provider-provider communication risks trouble many clinical settings, the consequences of missing or misunderstood test results can alter a provider’s diagnostic process and, potentially, set patients onto a dangerous trajectory.
- Technical Performance: A fifth of cases naming radiologists reflect substandard technical performance: this could involve operation of equipment, positioning of the patient, processing results, or other factors that resulted in a suboptimal procedure.
How to Protect Yourself and Your Patients
You can take a number of steps to mitigate the risk of an adverse event involving one of your patients.
- Create a Culture of Safety: Adopting and implementing communication best practices demonstrates to all radiologists, intradepartmental staff, and non-radiology colleagues that yours is a collaborative care environment that respects the need for clear results management and coordination of care.
- Technical Improvement: Clinical audits and other quality improvement efforts should pay particular attention to vulnerabilities exposed via MPL cases.
- Think Ahead: Many patients who allege medical malpractice against a radiologist point to breakdowns in communication of findings and the post-procedure care plan. An organizational assessment of test results management and communication can identify potential pitfalls, especially for high-impact results.
Learn More
By using the Candello data and best practices to drive your actions, you can close the gaps in your current processes. This will enhance a culture of safety for your patients and reduce your risk of being sued for malpractice.
- Emerging Risks in Interventional Radiology
- Navigating Risks in Breast Cancer Diagnosis and Treatment
- Miscommunication: Who, What, Where, When, How, and Why
- Malpractice Risks at the Front Line of Cancer Detection
Related Articles
What’s My Risk Library


Reducing the Occurrence of Malpractice Cases Involving Inadequate Patient Assessment

Risks in General Medicine: Contributing Factors