Newsletter
MPL Risks Associated with PAs
Jan 31, 2020
Approximately 110,000 physician assistants (PAs) were practicing in the United States as of 2016, with those numbers expected to grow by more than 30 percent over the next decade. Recent years have seen expansions in prescriptive privileges, scope of practice (including patient panels), and hospital admitting privileges. Concurrent with expanding their roles, PAs are increasing their medical professional liability (MPL) exposure.
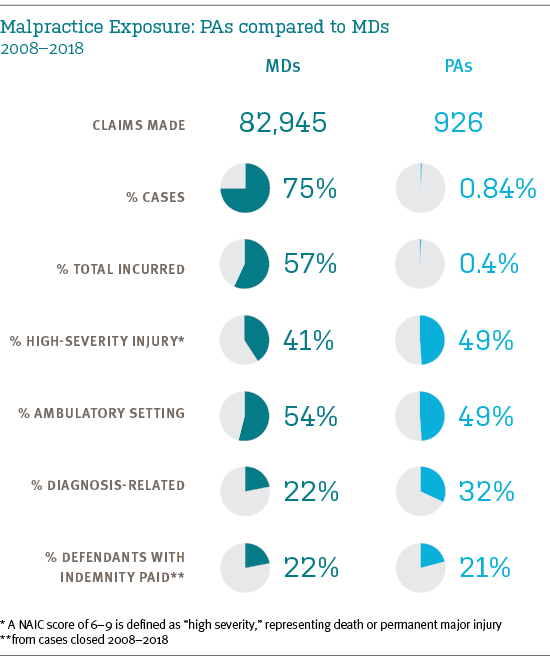
To see if their expanded liability exposure has triggered an increase in medical malpractice allegations, CRICO conducted an analysis of 110,000 MPL cases from across the U.S. The Comparative Benchmarking system (CBS) database was queried for cases in which a PA was a named defendant. Both cases opened and cases closed from January 1, 2008 to December 31, 2018 were analyzed. Over those 11 years, 926 CBS cases involved a PA. Extrapolated to the entire U.S., that equates to about 280 MPL cases per year naming a PA.
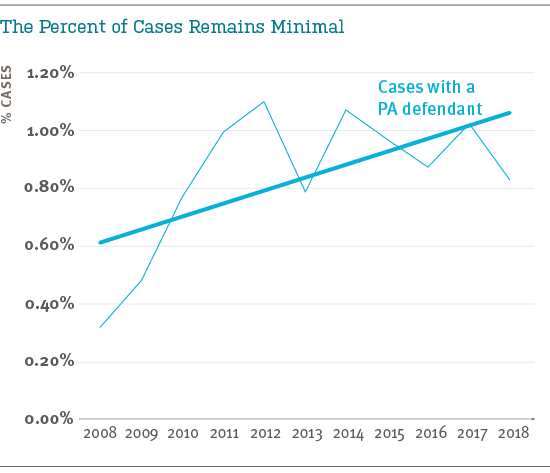
The cases naming a PA represent a small portion of all MPL claims and suits, with a slight upward trend from 2008–2012 that has leveled off more recently. In 57% of their cases, PAs are named along with a co-defendant.
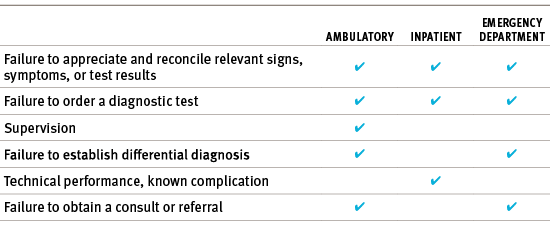
Half of all PA cases involve (non-emergency) outpatient care. In that setting, their primary vulnerability involves diagnosis-related events leading to severe injury (or death): 37% of PA cases from the ambulatory setting are diagnosis related, and 43% involve high-severity injuries. The key contributing factors seen in PA cases (across all care settings) are listed below.
In general, PAs are exposed to patient safety vulnerabilities similar to their physician colleagues. Organizations employing or insuring PAs can begin to identify opportunities to reduce exposure to situations that put patients—or other caregivers—at unnecessary risk, by considering the following questions:
- Is there clarity on scope of practice?
- Are accountable relationships based on unmodified state regulations, custom designed agreements, universal across all departments, or haphazard?
- Are there clear criteria for regular check-ins, escalation of care to a physician (e.g., patient factors or conditions that trigger MD involvement)?
- Are MDs and PAs educated about their malpractice liability, in particular regarding autonomous versus shared care?
- Do physicians within the organization believe PAs make them more vulnerable to malpractice allegations?
- Is the threshold for non-MD involvement in patient care extended indiscreetly?
- Are patients informed about the roles of PAs and their rights as patients?
- Is there team communication training in place?
Extending existing safety improvement programs to all members of patient care teams promotes a comprehensive understanding of risks, and greater likelihood that safety initiatives will be adopted and sustained.
References
A portion of the above content was previously published in the study Investigating MPL Vulnerability for the Institutions that Employ and Insure NPs and PAs, in the Aon/ASHRM Hospital and Physician Professional Liability Benchmark Analysis, October 2019 report.
- Bureau of Labor Statistics
- Kaiser Family Foundation State Health Facts: Physician Assistant Scope of Practice Laws
Additional Material
Recent Issues
Recently Asked Questions


At the End of Information Blocking, an Opening for Patient Safety
A Comparative Analysis of Nurse Practitioner, Physician Associate, and Physician Malpractice Risk

Characterizing Malpractice Cases Involving Emergency Department Advanced Practice Providers, Physicians in Training, and Attending Physicians

Inform Safer Medical Oncology Practice with Lessons from Medical Malpractice Claims

